Imagine being able to pre-screen for skin cancer in just seconds. That’s the aim of the DermR Patch, a new cancer screening test developed by Australian genomics researcher Stefan Mazy.
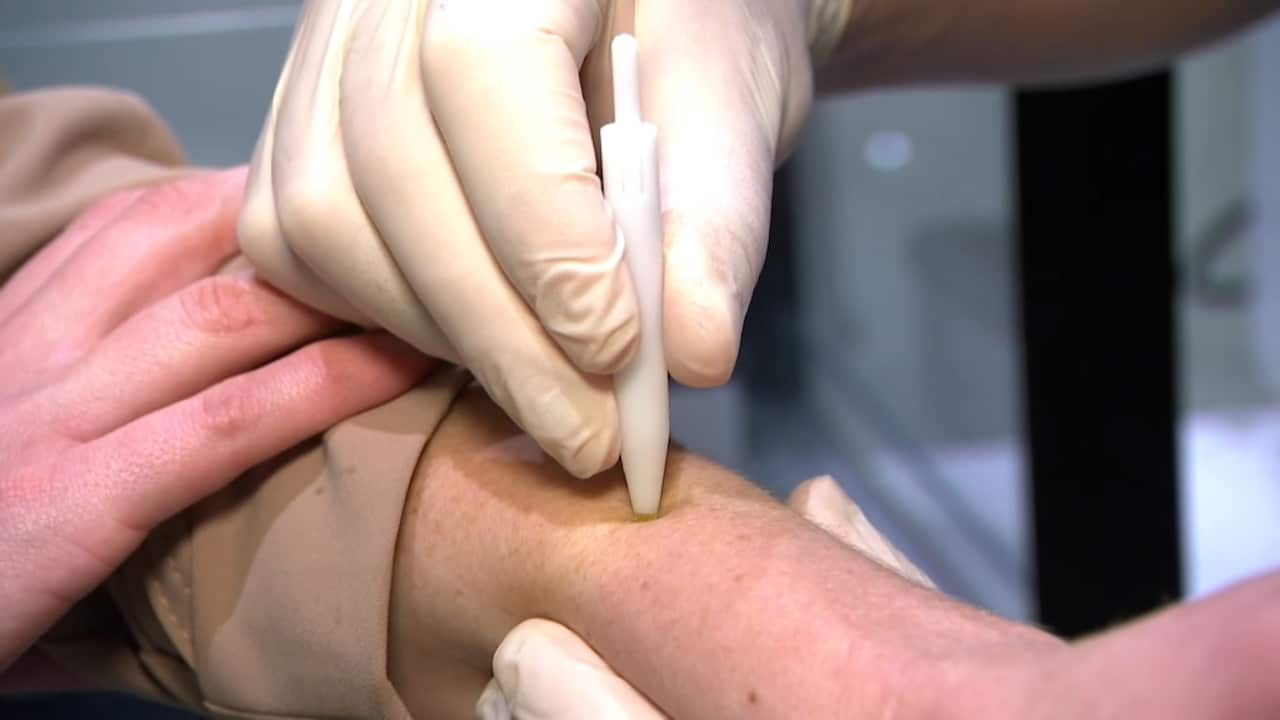
The first-of-its-kind technology harnesses the power of microneedles to identify cancerous lesions. The process is painless and quick.
“[The] microneedles are less than a millimetre long and they penetrate about a millimetre into the skin and they collect a micro amount of tissue,” Mazy explains.
“When we apply the patch, we put it on for about 15 seconds. There’s a little bit of pressure, there’s a slight twisting motion to get the tissue, [and] it then gets removed.
“The whole process takes under a minute. But the amount of tissue we collect is actually enough to perform a genomic analysis, which is highly sensitive. And using this methodology, we’re able to screen out which lesions could be potentially cancerous versus which ones we know have no cancer at all.”
Mazy developed the test with a team of four at DermR Health Solutions, the genomics company he founded and leads. Their first clinical trials took place in Western Australia’s remote Pilbara region in May.
While the final results are still pending, Mazy says early results look promising. The next step involves mounting a second and larger clinical trial, which is likely to happen within the next six to 12 months.
Stefan Mazy says the microneedles, which are less than a millimetre long, are painless. Source: SBS News / Abbie O’Brien
Inspired by mother’s diagnosis
Mazy developed the DermR Patch after his mother Gillian was diagnosed with basal cell carcinoma (BCC) which is a common form of skin cancer.
“[It] turned out to be quite aggressive and required surgical procedures to correct it. She went on to develop life-long sleep apnea due to the surgery,” Mazy says.
Gillian, who was born in Mauritius, initially put off having a biopsy for the lesion on her nose because she was scared of needles. She also didn’t believe she was at risk of developing skin cancer because of her Mauritian background.
Mazy describes his mother’s delayed diagnosis as “quite traumatic”.
“Nobody really expects something so little as a lesion to have such a profound effect,” he says.
“All of this could have been avoided if there was another way to test for skin cancer without a needle or an incision.”
Stefan Mazy developed the skin patch after his mother, Gillian, was diagnosed with basal cell carcinoma. Credit: Supplied
‘No pain, no bleeding, no cutting’
Mazy’s hope is that the DermR patch could one day be an alternative to a biopsy, which is the most common method for diagnosing skin cancer.
Compared with the patch test, biopsies are more invasive and take longer. The procedure is typically carried out by a GP with the use of a local anaesthetic.
WA-based dermatologist Dr Stephanie Weston explains: “It involves taking a small sample of skin [and] sending it off to the laboratory. So there’s a small wound there that has to heal.”
“It is a minor procedure, but it is a procedure.”
Weston is a fellow of the Australasian College of Dermatology and says not all GPs are trained to perform biopsies, which can lead to increased wait times for diagnoses.
If clinical trials of DermR are successful, the microneedle patch could offer patients a more accessible and far less invasive option for screening.
“There’s no pain, no bleeding, no cutting,” Mazy says.
He believes it could also be useful for diagnosis in remote and regional areas, where access to GPs can be limited.
“One of the biggest barriers that we face are the skill shortages — in particular, doctors. So where we feel our solution has the perfect fit is that [the patch test] can enable nurses and allied health providers to be able to administer a biopsy-equivalent diagnostic test,” he says.
While the patch test could replace biopsies at the screening stage, Mazy says, patients who show signs of cancer will still require a follow-up biopsy.
“I guess the whole idea is to triage, so [deciding] which patients do need to get medical attention and which patients don’t.”
One of the biggest barriers that we face are the skill shortages — in particular, doctors. So where we feel our solution has the perfect fit is that [the patch test] can enable nurses and allied health providers to be able to administer a biopsy-equivalent diagnostic test.
Stefan Mazy, genomics researcher
Skin cancer capital of the world
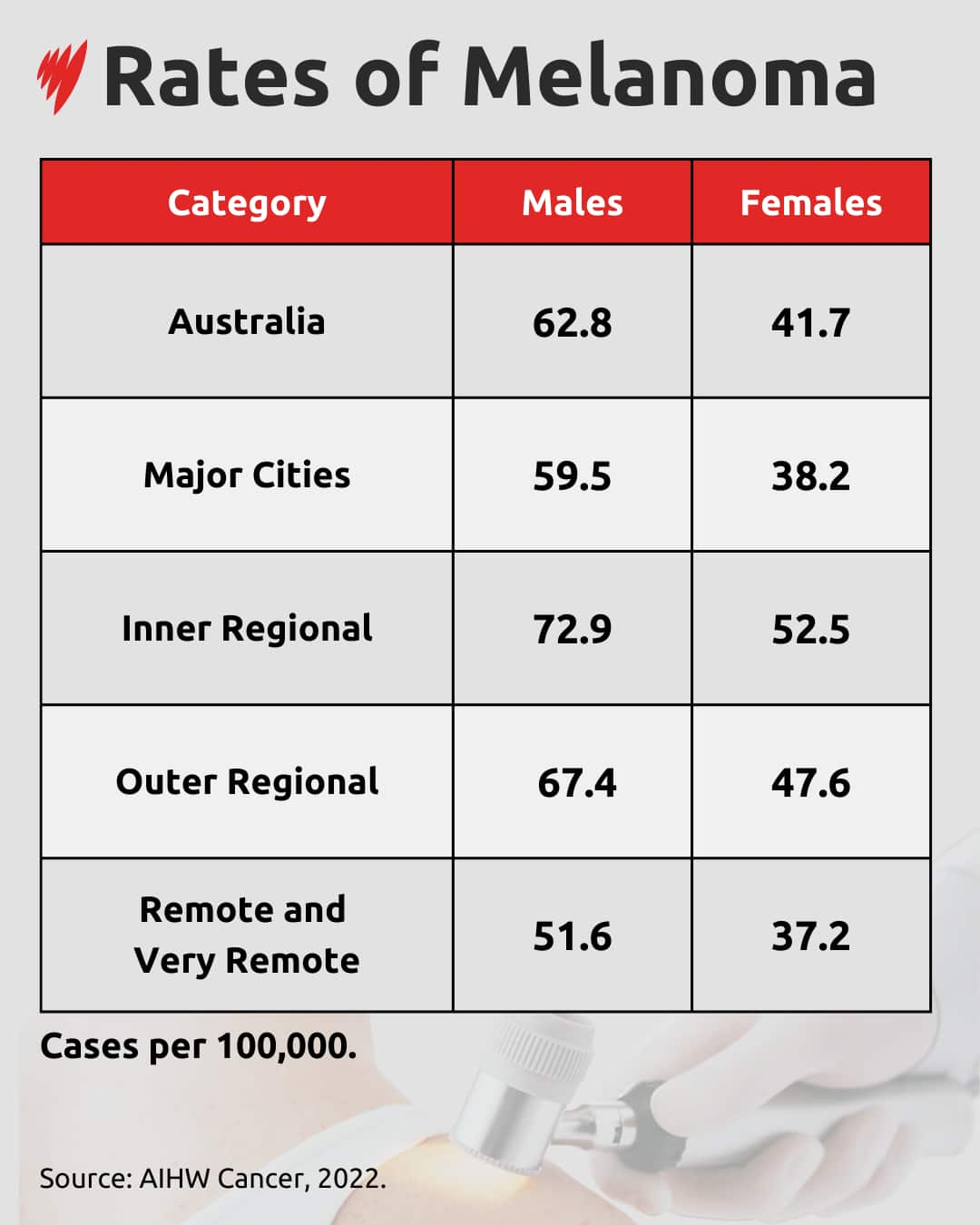
Australia is often dubbed the “skin cancer capital of the world”, due to record-high rates of melanoma and other forms of skin cancer.
According to the Cancer Council, around two-thirds of Australians will be diagnosed with some form of skin cancer during their lifetime.
Regional Australians are more at risk compared with those who live in major cities. At the same time, access to healthcare — including skin checks — can be limited in regional areas.
“[In] rural and regional Australia, we know we carry a significant burden of skin cancers,” says Dr Nicole Higgins, president of the Royal Australian College of General Practitioners.
“The access to specialised skin cancer services is reduced. That being said, it’s also the bread-and-butter work of rural GPs.”
Higgins is based in Mackay in regional north Queensland and says a wider range of solutions for regional Australians is needed.
“Anything that improves access and reduces costs for patients is something that we’re all aiming for. And if we can get technology that makes it easier and causes less pain, that’s always a good thing,” she says.
A graphic card showing rates of Melanoma. Source: SBS News
According to the Melanoma Institute Australia, 90 per cent of melanoma cases can be successfully treated with surgery if detected early.
But there are barriers to early detection for regional and rural Australians.
Registered nurse Jessica Evans, who works in remote areas of WA, says a lack of access to specialised care can prevent people from getting a skin check.
“In a lot of the areas up in the Pilbara, we either have limited doctors or no doctors, [and] doctors that don’t necessarily specialise in skin or thorough skin checks,” she says.
The DermR patch is currently being tested in the Pilbara and could eventually be rolled out to other remote and regional areas if it is successful.
Professor Pascale Guitera is a dermatologist at the Melanoma Institute Australia and the director of the Sydney Melanoma Diagnostic Centre at Royal Prince Alfred Hospital. She says this kind of technology “will be the way of the future”.
“It’s great because of the equity, in terms of access to all the patients through a nurse, for example,” she says.
But she says it’s still early days and melanoma diagnoses can be “complex”.
“We don’t know yet about the costs, for example, or the accuracy. We have a lot of diagnoses that are not white or black — they’re grey. So they need a lot of skill and experience from the doctor.
“But of course, I wouldn’t say because it’s complex, we should not try.”
The microneedles penetrate about a millimetre into the skin and collect a tiny amount of tissue. Stefan Mazy says the process takes about 15 seconds. Source: SBS News / Abbie O’Brien
For Weston, who runs regional outreach clinics and is the visiting dermatologist at the Karratha Health Campus in the Pilbara, the DermR Patch is an exciting prospect for regional communities.
She says, if successful, the DermR Patch could be a “really useful diagnostic tool”.
“If you’re a country patient and you have a simple sort of investigative technique and it says, ‘Actually this is skin cancer’, then you can prioritise the next step.
“[Patients can say], ‘Right, well I was planning on going [for a check] in six months’ time, but actually now I’ll bring that forward’. Or you might get the reassurance that this one isn’t something that needs to be treated in the next week or two, so that appointment in six months will be fine.
“I think this is a really exciting time to be in medicine.”