An estimated 3.6 million Medicare beneficiaries could potentially access Wegovy now that the Food and Drug Administration (FDA) approved the drug for reducing the risk of incidents related to cardiovascular disease.
A KFF analysis found that among the 13.7 million people on Medicare diagnosed with obesity, 3.6 million, or roughly 1 in 4, of these beneficiaries also have diagnoses of cardiovascular disease. These potential beneficiaries represent about 7 percent of all those on Medicare.
These findings are based on data from 2020.
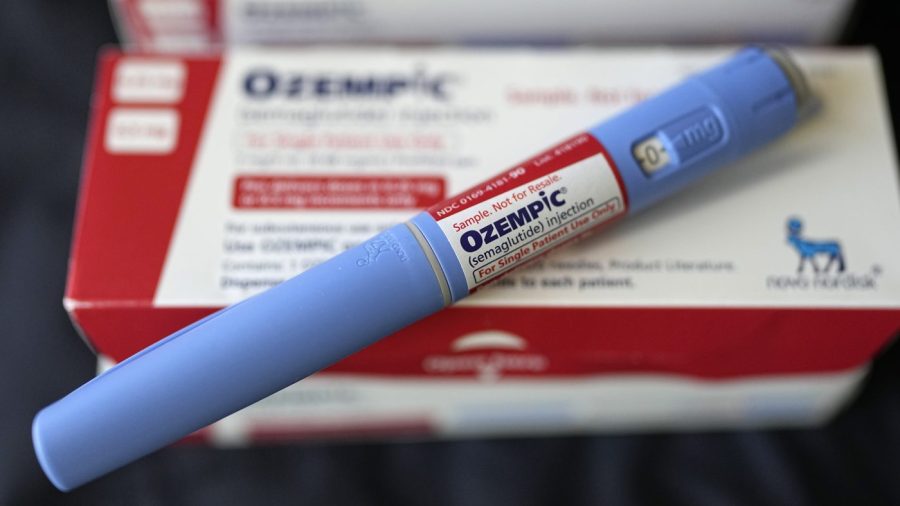
Wegovy is a form of semaglutide, also sold as the diabetes treatment Ozempic. As GLP-1 agonist, it is among the class of drugs that have until recently only been approved to treat diabetes and obesity.
Medicare is prohibited from covering weight loss medications due to the Medicare Modernization Act of 2003. Lawmakers, pharmaceutical manufacturers and obesity care specialists have been pushing to change this by calling for the passage of the Treat and Reduce Obesity Act (TROA) that would allow for obesity medications and other related services to be covered.
KFF’s analysis also projected the possible cost in covering Wegovy. The policy nonprofit estimated that if just 10 percent used Wegovy in a given year, Medicare would incur almost an extra $3 billion in Part D spending.
“If more Medicare beneficiaries with obesity or overweight gain access to GLP-1s based on other approved uses for these medications, that could reduce the cost of proposed legislation to lift the statutory prohibition on Medicare coverage of anti-obesity drugs,” KFF’s analysis read.
Beneficiaries would also see potential out-of-pocket costs ranging from $325 to $430.
The FDA granted Wegovy approval last month for reducing the risk of cardiovascular death, heart attack and stroke in patients with cardiovascular disease and obesity. The agency cited results from a multinational study conducted by Novo Nordisk, the manufacturer of Wegovy, that found the drug reduced the risk of major adverse cardiovascular events by 20 percent.
The mechanism of action for this reduction was not established in the study.
As a healthcare professional, I believe it is crucial for Medicare to reconsider its coverage ban on weight loss medications like Wegovy. The potential health benefits for beneficiaries with obesity and cardiovascular disease could be significant, and access to such treatments can ultimately lead to better outcomes and reduce healthcare costs in the long run.
As a healthcare professional, I believe it’s crucial for Medicare to adapt and cover weight loss medications like Wegovy for beneficiaries with obesity and cardiovascular disease. Expanding coverage will undoubtedly lead to better health outcomes and potentially reduce healthcare costs in the long run.